Dr. Ria Kyriakidou Savvidou: Is Vaccination Against HPV Important?
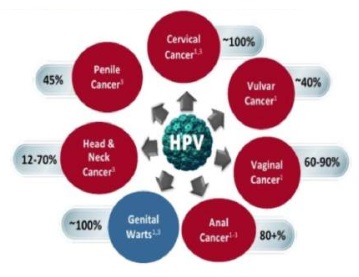
The HPV virus is a very common virus and belongs to the large family of DNA viruses, that of human papillomavirus (Human Papilloma Viruses). It is capable of causing infections, genital warts, precancerous lesions and cancer in the proctogenic area and in the oropharyngeal area, as well as in the head of both men and women. It can be very easily transmitted through genital contact, by penetration or not, orally, genitourinary, perinatal contact and rarely during childbirth. In children, transmission mainly occurs directly from person to person and indirectly from infected objects and surfaces.
Both men and women can remain asymptomatic for many years, as the immune system of healthy carriers supresses the onset of the infection. However, during their lifetime, about 80% of sexually active women and 50% of sexually active men may develop an infection.
Cervical cancer is the 2nd leading cause of death in women worldwide. The highest mortality rates (88%) are observed in low-income countries (Sub Saharan Africa, South and Central Asia, South America). More than half a million of women worldwide develop cervical cancel each year, and 275,000 of them lose the fight.
Within the next 65 years, and if current trends in social life remain the same, the results will be devastating. An alleged scenario of non-vaccination of people is expected: 65 million new cases of cervical cancer and 10 million deaths in women between the age of 10 and 29.
Protection
As barriers to this destructive course are now two important tools of science: the discovery and production of vaccines against HPV and the implementation of organized screening health programs.
The main goal is primarily prevention, with early vaccination of both genders, prior to exposing them to the risk of being infected with the onset of sexual activity. Ages between 9 and 26 are ideal, due to a greater stimulated immune system. This does not preclude older age groups, as vaccination develops antibodies to a satisfactory degree of protection.
The vaccine owes its success to that it is a non-infectious recombinant vaccine prepared from the purified virus-like particles (VLPs) of the major capsid (L1) version of various HPV types. By introducing them into the body, they mimic the structure of the native virus, causing production of neutralised antibodies for long term protection. In other words, they do not contain viral DNA, they are not live attenuated viruses and, therefore, cannot cause active infection.
The upgraded 9-valent vaccine is the newest prevention tool. The ten-year global experience and the results of the precursor, the 4-valent vaccine, led to the production of the 9-valent vaccine which contains even more oncogenic types for greater protection against cervical cancer, as well as other HPV-related precancerous lesions and vulvar, vaginal and anus cancer. The protection rate reaches that of 97%.
PAP TEST’s cytological screening remains a valuable tool for symptomatic screening. It aims to detect potentially precancerous and cancerous lesions of the cervix, but does not prevent them from occurring due to a possible previous infection. In case of pathological results from a PAP TEST, it is recommended to identify the strains of the virus with an HPV/ DNA TEST. Both test are secondary prevention. Internationally, the diagnostic sensitivity of the PAP TEST is around 75% and 93 – 96% for the HPV/ DNA TEST.
Combining those two gives satisfactory diagnostic rates but not sufficient. Although the human papillomavirus (HPV) is the most common venereal disease, there is no radical cure for it.
The priority of modern man and woman should be to strengthen their body with the most “powerful weapons” before cancer occurs. The best prevention is primary prevention. Vaccination with the 9-valent is the safest and most effective method for fighting cancer.
Dr. Ria Kyriakidou Savvidou
Obstetrician - Gynaecologist Surgeon